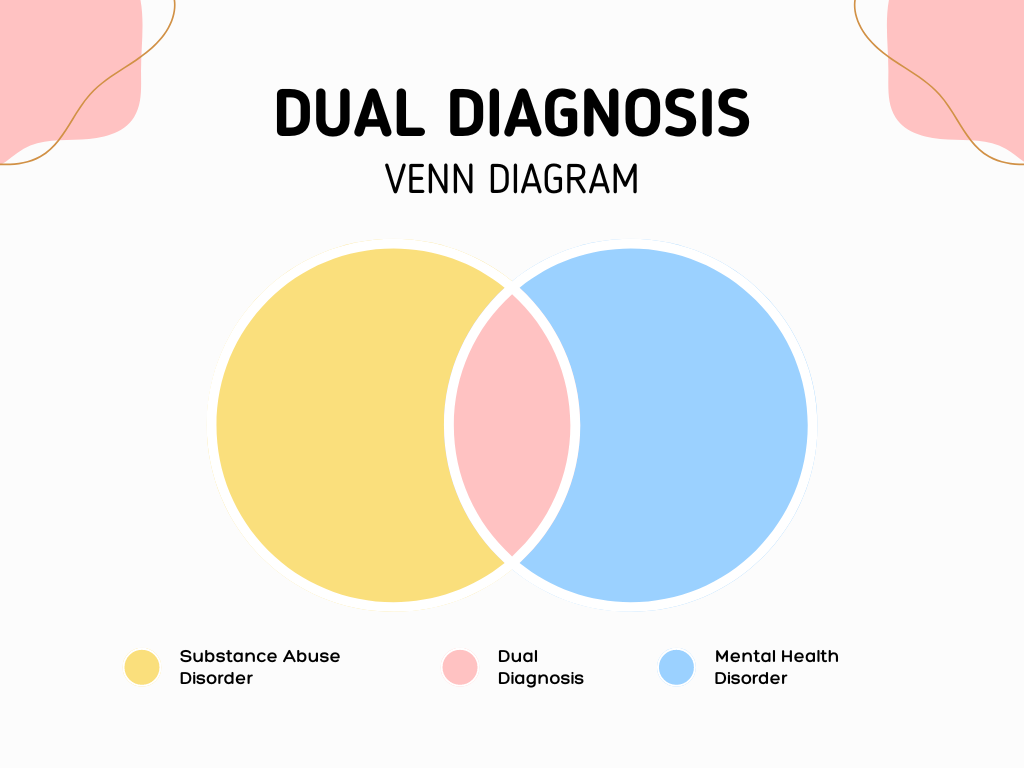
Dual diagnosis, also known as co-occurring disorders, refers to the simultaneous presence of a mental health disorder and a substance use disorder. This complex interplay poses significant challenges for individuals, healthcare providers, and public health systems. In the UK, USA, and Canada, dual diagnosis is a prevalent issue that requires comprehensive and integrated treatment approaches. This post explores the prevalence, challenges, and treatment strategies for dual diagnosis in these three countries.
Understanding Dual Diagnosis
Dual diagnosis involves a wide range of mental health disorders, including depression, anxiety, bipolar disorder, schizophrenia, and post-traumatic stress disorder (PTSD), occurring alongside substance use disorders involving alcohol, drugs, or both. The relationship between these conditions is bidirectional: mental health issues can lead to substance abuse as individuals may use drugs or alcohol to self-medicate, and conversely, substance abuse can exacerbate or trigger mental health disorders.
Prevalence in the UK
In the UK, dual diagnosis is a significant public health concern. The National Institute for Health and Care Excellence (NICE) estimates that around 30-50% of individuals with severe mental health problems also experience substance use disorders. According to Public Health England, approximately one-third of people in drug and alcohol treatment services have a concurrent mental health condition.
Prevalence in the USA
In the USA, the Substance Abuse and Mental Health Services Administration (SAMHSA) reports that approximately 9.5 million adults had both a mental health disorder and a substance use disorder in 2019. This represents about 3.8% of the adult population. The National Institute on Drug Abuse (NIDA) highlights that individuals with mental health disorders are twice as likely to suffer from substance use disorders compared to the general population.
Prevalence in Canada
In Canada, the Canadian Centre on Substance Use and Addiction (CCSA) indicates that about 20% of individuals with a mental health disorder also have a substance use disorder, and vice versa. The prevalence of dual diagnosis is particularly high among marginalized populations, such as the homeless and incarcerated individuals. Statistics Canada reports that around 21% of people with a mood or anxiety disorder also have a substance use disorder.
Challenges of Dual Diagnosis
Dual diagnosis presents numerous challenges for individuals and healthcare providers:
- Complexity of Symptoms: The symptoms of mental health disorders and substance use disorders can overlap, making diagnosis and treatment more complicated. For example, substance use can mask or mimic symptoms of mental illness, leading to misdiagnosis or underdiagnosis.
- Stigma and Discrimination: Individuals with dual diagnosis often face significant stigma and discrimination, which can deter them from seeking help. This stigma is prevalent both within society and within healthcare systems, where providers may lack the training or willingness to address co-occurring disorders.
- Access to Integrated Care: Traditional treatment models often separate mental health and substance use services, resulting in fragmented care. Integrated treatment, which addresses both conditions simultaneously, is essential but not always readily available.
- Relapse Risk: The presence of dual diagnosis increases the risk of relapse for both substance use and mental health disorders. The interplay between these conditions can create a cycle where the treatment of one disorder is undermined by the symptoms of the other.
- Social and Economic Factors: Socioeconomic factors, such as poverty, unemployment, and lack of social support, can exacerbate both mental health and substance use disorders. These factors are often prevalent among individuals with dual diagnosis, further complicating their recovery.
Treatment Approaches
Effective treatment for dual diagnosis requires a comprehensive and integrated approach that addresses both mental health and substance use disorders simultaneously. Key components of treatment include:
- Integrated Treatment Programs: These programs combine mental health and substance use treatment within a single, cohesive framework. Integrated treatment has been shown to improve outcomes by providing consistent, coordinated care.
- Medication-Assisted Treatment (MAT): MAT involves the use of medications, such as antidepressants, antipsychotics, or medications for opioid use disorder (e.g., methadone, buprenorphine), alongside behavioral therapies. MAT can help manage symptoms, reduce cravings, and support recovery.
- Cognitive Behavioral Therapy (CBT): CBT is effective for treating both mental health and substance use disorders. It helps individuals identify and change negative thought patterns and behaviors, develop coping strategies, and manage triggers.
- Motivational Interviewing (MI): MI is a counseling approach that enhances motivation to change by exploring and resolving ambivalence. It is particularly useful for individuals who may be hesitant or resistant to seeking treatment.
- Peer Support Groups: Peer support groups, such as Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and mental health support groups, provide valuable social support and a sense of community. These groups can help individuals stay motivated and connected during recovery.
- Case Management: Case management involves coordinating care and services to address the complex needs of individuals with dual diagnosis. This includes connecting individuals to housing, employment, legal assistance, and other support services.
- Holistic Approaches: Holistic approaches, such as mindfulness, yoga, and exercise, can complement traditional treatments by promoting overall well-being and stress reduction.
Dual Diagnosis in the UK
In the UK, addressing dual diagnosis involves a combination of national guidelines, specialized services, and local initiatives. NICE provides comprehensive guidelines for the treatment of co-occurring mental health and substance use disorders, emphasizing the need for integrated care. The NHS has developed specialized dual diagnosis services, although access can vary by region.
Public Health England has implemented initiatives to improve coordination between mental health and substance use services. Local initiatives, such as the London Dual Diagnosis Network, aim to share best practices and improve service delivery for individuals with dual diagnosis.
Dual Diagnosis in the USA
In the USA, SAMHSA promotes integrated treatment through its Co-Occurring Disorders Program. SAMHSA’s TIP 42 provides best practice guidelines for treating co-occurring disorders, emphasizing the importance of integrated care, culturally competent services, and evidence-based practices.
The Affordable Care Act (ACA) has expanded access to mental health and substance use treatment by requiring insurance plans to cover these services. Despite this, access to integrated care remains inconsistent, with rural areas and marginalized populations facing significant barriers.
Dual Diagnosis in Canada
In Canada, the CCSA and provincial health agencies work to address dual diagnosis through integrated treatment models and public awareness campaigns. The Mental Health Commission of Canada (MHCC) advocates for improved access to mental health and substance use services, emphasizing the need for coordinated care.
Provinces such as Ontario and British Columbia have developed specialized programs to address dual diagnosis, focusing on integrated treatment, peer support, and case management. However, access to services can still be challenging, particularly in rural and remote areas.
Conclusion
Dual diagnosis is a complex and challenging issue that requires comprehensive, integrated approaches to treatment. In the UK, USA, and Canada, significant efforts are being made to address the needs of individuals with co-occurring mental health and substance use disorders. Despite these efforts, barriers such as stigma, fragmented care, and limited access to services remain.
By promoting integrated treatment models, enhancing access to care, and addressing the social determinants of health, we can improve outcomes for individuals with dual diagnosis. Public awareness campaigns and advocacy efforts are also essential to reduce stigma and ensure that individuals with co-occurring disorders receive the support and care they need.